MIT engineers have developed advanced liver tissue models that more accurately mimic human liver architecture and disease states, offering new ways to test treatments for metabolic dysfunction-associated steatotic liver disease (MASLD) and related conditions.
Researchers at MIT have created sophisticated new tissue models that could revolutionize how scientists develop treatments for liver disease, offering more accurate ways to test potential drugs before they reach human trials.
The team, led by Professor Linda Griffith, has developed two distinct approaches to modeling liver tissue that better replicate the complex architecture and physiology of the human liver. These advances could help address the growing global burden of metabolic dysfunction-associated steatotic liver disease (MASLD), which affects more than 100 million people in the United States alone.
A more realistic liver-on-a-chip
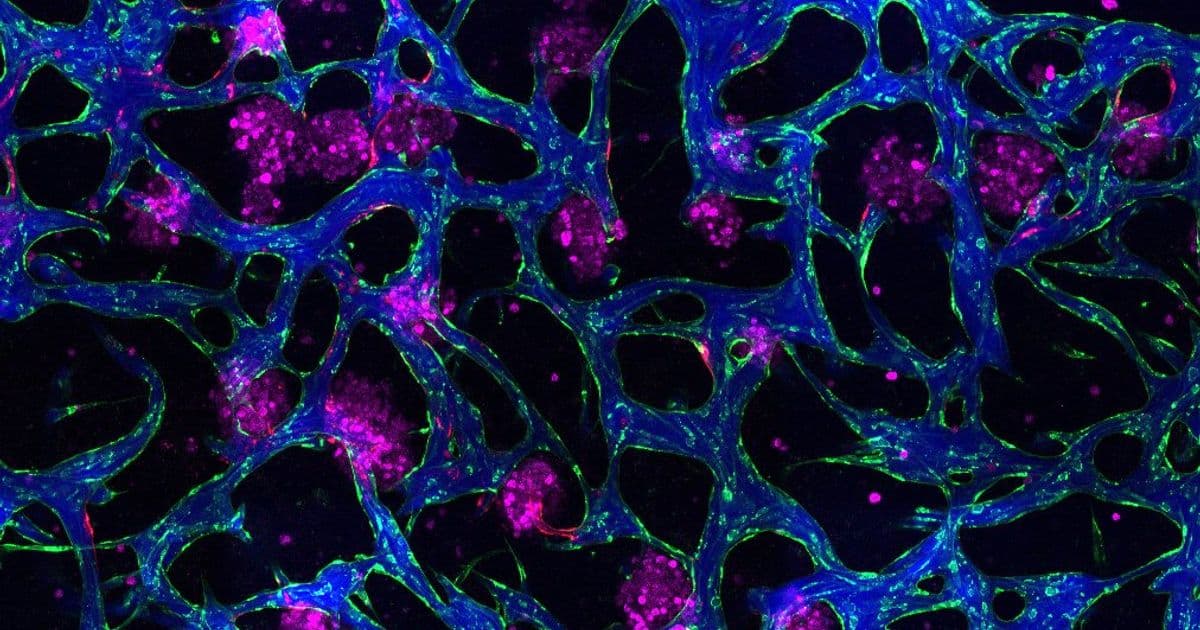
The first breakthrough, detailed in a paper published today in Nature Communications, involves a new type of microfluidic device that creates a more realistic liver tissue model. The key innovation is the incorporation of blood vessels that can carry fluid and allow immune cells to flow through the tissue.
In this system, tiny clusters of liver cells are embedded within a network of blood vessels. As shown in the accompanying time-lapse video, immune cells called monocytes can move through these vessels, with some gathering around liver cell clusters while others leave the vessels and enter the surrounding tissue. This mimics the increased immune cell infiltration commonly seen in liver disease.
"The real advance here was showing that we could get an intimate microvascular network through liver tissue and that we could circulate immune cells," Griffith explains. "This helped us to establish differences between how immune cells interact with the liver cells in a type two diabetes state and a healthy state."
The researchers demonstrated that their model could accurately replicate the inflammation and metabolic dysfunction that occur in early-stage liver disease. When they induced insulin resistance by exposing the tissue to elevated levels of insulin, glucose, and fatty acids, they observed changes in how liver cells clear insulin and metabolize glucose, as well as narrower, leakier blood vessels that reflect microvascular complications often seen in diabetic patients.
Unexpected findings with existing drugs
In a related study published in Communications Biology on January 14, the team used an earlier version of their liver tissue model to investigate how the liver responds to resmetirom, a drug currently used to treat metabolic dysfunction-associated steatohepatitis (MASH), an advanced form of liver disease.
Resmetirom works by mimicking the effects of thyroid hormone, which stimulates the breakdown of fat. However, it's only effective in about 30 percent of patients. The researchers discovered that the drug can induce an inflammatory response in liver tissue, which may help explain why it doesn't help all patients.
"Because resmetirom is primarily intended to reduce hepatic fibrosis in MASH, we found the result quite paradoxical," says Dominick Hellen, the lead author of that study. "We suspect this finding may help clinicians and scientists alike understand why only a subset of patients respond positively to the thyromimetic drug."
Building better disease models
The motivation behind these studies stems from the limitations of current approaches to drug development for liver disease. While existing tissue models can predict liver toxicity for certain drugs, they don't adequately model disease states where researchers need to identify drug targets and validate their effectiveness.
"There are already tissue models that can make good preclinical predictions of liver toxicity for certain drugs, but we really need to better model disease states, because now we want to identify drug targets, we want to validate targets," Griffith says. "We want to look at whether a particular drug may be more useful early or later in the disease."
To create their MASLD model, the researchers exposed liver tissue to high levels of insulin along with large quantities of glucose and fatty acids. This led to a buildup of fatty tissue and the development of insulin resistance, traits commonly seen in MASLD patients and which can lead to type 2 diabetes.
The research team includes Erin Tevonian PhD '25 and Ellen Kan, both from the Department of Biological Engineering, who are lead authors of the Nature Communications paper, along with former MIT postdoc Dominick Hellen, lead author of the Communications Biology paper.
The broader context
This work represents part of a larger effort by Griffith's lab to use microphysiological systems to explore human liver biology, which cannot be easily replicated in mice or other animals. The team's approach builds on the LiverChip, a microfluidic device that Griffith originally developed in the 1990s and which is now widely used by pharmaceutical companies to test whether new drugs have adverse effects on the liver.
The research was funded by the National Institutes of Health, the National Science Foundation Graduate Research Fellowship program, NovoNordisk, the Massachusetts Life Sciences Center, and the Siebel Scholars Foundation.
These advances come at a critical time, as liver disease continues to be a major global health challenge. With only two FDA-approved medications currently available for MASH, finding new treatments is a priority. As Griffith notes, "You're never declaring victory with liver disease with one drug or one class of drugs, because over the long term there may be patients who can't use them, or they may not be effective for all patients."
The new tissue models offer researchers powerful tools to better understand liver disease mechanisms and test potential treatments in more realistic human tissue environments, potentially accelerating the development of new therapies for millions of patients worldwide.
Comments
Please log in or register to join the discussion